Diastasis Recti Abdominis
Every time I sit up in the bed and notice a bubble in the middle of my stomach?
There’s a soft spot in the middle of the belly. What is it???
I have a mama pooch!!
I feel like I'm not strong through the core and have a hard time twisting or picking something up without the belly feeling funny?
General anatomy:
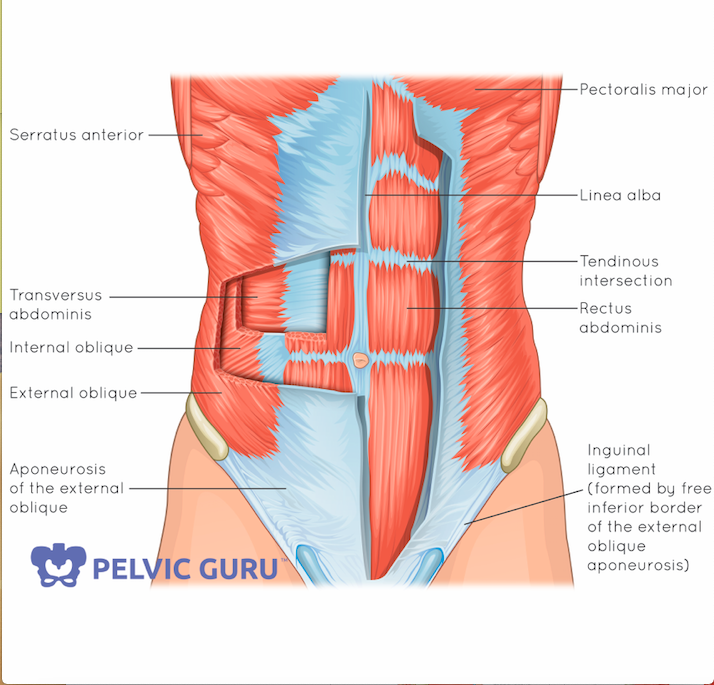
Layers of abdominal muscles - all connect at the linea alba in the middle.
Normal Anatomy - the abdomen has layers of muscles - the transverse abdominis runs horizontally, the internal and external oblique's form an “x” and then the rectus abdominis running up and down (known as your 6-pack muscles). They all connect in the middle through the linea alba which is a connective tissue or fascia connecting the right and left of the abdominal muscles.
The abdominal muscles are just a portion of the “core” that is important with moving, lifting, and all our functional activities even breathing. Because of this, when the muscles or fascia are not working optimally, it can lead to other issues. One such issue being a Diastasis Recti abdominis.
What is DRA?
A diastasis recti abdominis (DRA) is where the belly muscles, or most obviously the rectus abdominis, separates. The line in the middle of the abdomen is called the linea alba which is a fascia or connective tissue that holds both sides of the abdominal muscles together. It is said that up to 100% of women have this soften or stretch to allow for growth of a baby during the last trimester of pregnancy which is a normal part of pregnancy. In fact, it is so common most people don’t realize they have it until after delivery when they realize their belly still looks different from pre-pregnancy. A DRA can be in different sections of the belly as well and the most common is just slightly in the middle along the whole length.
Who is at risk?
Once again there are no black and white answers for this and some women can have one of these factors but not ever have issues. Men can even have a diastasis.
Some studies show that
pregnancy,
multiple pregnancies,
C-sections,
abdominal surgery (laparoscopic surgeries, gallbladder removal etc),
people who have conditions where their collagen is not as strong (Ehlers-Danlos syndrome or other issues with laxity),
large changes in body mass (people who have a gastric bypass surgery)
Other contributing factors include poor posture, poor breathing habits, poor lifting habits, poor bowel or bladder habits, and/or not resting enough immediately after delivery.
How do I know if I have one?
What do I do if I think I do have a DRA?
There are no definitive answer and no specific research to support a specific program but some research says exercise in general will help reduce the occurrences. Others studies suggest there is no difference with occurrences for those who exercise during and before pregnancy. A physical therapist is trained to assess all aspects of the core to determine where there may be deficits. This is why it is so complicated - there are so many There are no blanket rules for what to avoid - some women can do planks and other "harder" exercises while others stop during 1st or 2nd trimester. Watching how the belly is able to control your movements is key as well as other symptoms you may be noticing like incontinence, having to hold your breath, or pain.
HOWEVER -
It is often recommended to reduce the load on the abdominal wall and pelvic floor as the baby and abdomen grow.
Avoiding the "doming" of the abs is recommended too
What about abdominal Bracing, binding or compression wraps
Mixed research on this too for postpartum wraps - some think it helps support the abs, organs, lumbar spine, reduce tension on linea alba, reduces swelling and adds compression for more confidence and comfort. - no definitive research - some think it adds more pressure to the system and can push more on the PFM or weaken the core by not making it too dependent.
Use a brace/wrap if you
not able to rest during the first few weeks postpartum
have pain in the back, pelvis, pubic symphysis
need support for C-section incision
have a 3 finger width separation or wider
are doing higher level exercises and feel you need it (though most women's health physical therapists would suggest against this as you should get yoru body stronger without support)
What does research say?
One article showed that out of 300 women, 12 months after delivery 34% still had a diastasis of 2 fingers. This is unfortunate because most mothers go into a second or third pregnancy with a predisposition to weakness and thus more tension and thinning to the linea alba. Awareness is key and so is proper diagnosis.
There is poor agreement as to the size of the separation that may be pathologic (or cause problems in the long term) and there is no apparent association between pre-pregnancy body mass index, weight gain, baby's birth weight, heavy lifting, and regular exercise. Research also refutes the suggestion that a DRA would lead to low back pain, pelvic pain, or pelvic floor dysfunction but when you understand the pressure system in the body - how can you not have 1/4 of the canister working properly and not predispose the other 3 to an issue?
Narrowing of the gap is not the only way we determine healing has taken place - How one creates tension between the 2 sides and activate your deep core seems to be one of the best ways to treat. It all depends on what the activity is, how the individual performs it and the form in which it's performed.
Even though a gap may be closed with the test - function is what is needed and you can still have a gap without losing function or feel weak
Healing can depend on time, age, number of pregnancies, genetics, and size of babies
The best exercises are pilates teaching how to fire with the transversus abdominis AND rectus abdominis, manual therapy to help improve fascia and alignment, postural corrections, breathing improvement, lifting techniques and the Noble technique (pulling the muscles together with your hands while doing a crunch type movement).
The best treatment is one tailored to YOUR abilities. Having someone WATCH you and assess your daily activities can make a huge difference. It's difficult for a lot of us to see ourselves especially during the day and with real life things (like putting kids in the tub, car or even lifting groceries).
Don’t mistake a diastasis for a hernia.
Sometimes a medical professional is not able to tell the difference between a true diastasis and a hernia. It is not always a "rush-to-the-doctor" matter and may improve with core retraining as well. A hernia is when the abdominal contents start to push out of a small hole in the abdominal wall or fascia. A hernia is concerning when there is discoloration of the tissue, pain that changes with eating patterns, or vomiting. We are not certain of the prevalence of umbilical hernias or abdominal hernias but a lot of women have them postpartum. Our belly button (umbilicus) is a weakening of the abdominal wall from birth and it's suspected that with the stretching for pregnancy it just further weakens.
When to seek a Physical Therapist?
When your diastasis is 3 finger widths or more or a big bulge between your abdominals or deeper than 1 cm
When you are not sure where to start
When you have back pain and/or pelvic floor symptoms
When you cannot create tension or don’t know how
When there are multiple symptoms that are difficult to navigate with a trainer/instructor